Cranioplasty refers to the operation of filling and repairing the defective skull with various repair materials. It is currently one of the most routine neurosurgery operations and can be carried out in many primary hospitals. Studies have proved that cranioplasty not only restores the shape of the cranial cavity, but also achieves the effect of restoring aesthetics, and also plays an important role in the recovery of the patient's neurological function.
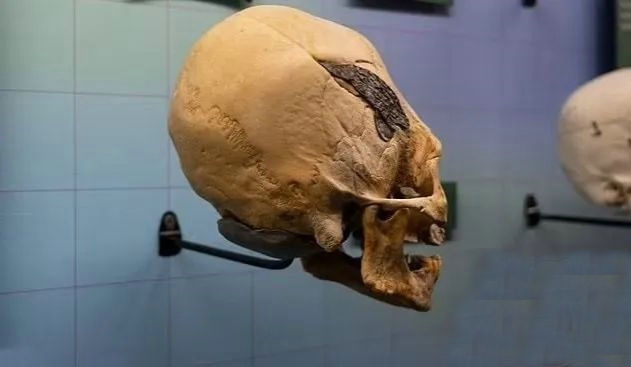
Cranioplasty is a medical technique with a long history. Our ancestors had already carried out such medical attempts thousands of years ago. The Museum of Osteology in Oklahoma, USA has a collection of a warrior in Peru 2,000 years ago The warrior's skull was injured in battle, and a metal plate was implanted in the wound to repair the fracture.
With the rapid development of industrial level, science and technology, and diagnosis and treatment methods, cranioplasty has become a relatively common and routine operation in neurosurgery. During this process, cranioplasty materials also go through the following stages:
Xenograft bone material
In 1668, doctor van Meekeren used canine bone tissue to repair a human skull defect, which was the first documented xenograft in the world. Subsequently, the use of bone tissues such as apes, rabbits, and cattle to be transplanted to humans appeared one after another. In addition to common complications such as post-transplant infection and bone resorption, xenograft bone transplantation often causes secondary damage to patients due to the great immune rejection of xenograft materials by the human body.

Autologous bone graft
In 1821, doctor Vonwalther performed the world's first autologous bone graft to repair skull defects. In 1867, doctor Lollier proposed the important role of periosteum in bone regeneration. Subsequently, there have been a large number of reports in the literature on the repair of skull defects with autologous skull flaps, mandibular outer plates, ribs, iliac crests, and fibula flaps. Autologous ribs made into strips or powder are suitable for repairing small skull defects. At present, autologous bone repair is still the gold standard for skull reconstruction. Autologous bone tissue has good osteoconductivity and histocompatibility, no rejection, and a low rate of postoperative bone exposure. Increased secondary trauma, high bone resorption rate of grafted bone and other problems, the clinical application is limited.
Allograft bone
The large numbers of soldiers in World War I and World War II who suffered skull defects from gunshots and explosions led to significant advances in methods of repairing skull defects. At the beginning of the 20th century, there were reports of using human cadaver skull transplantation to repair skull defects. Allograft materials are often obtained from other people's bone flaps, which can solve the problem of insufficient autologous bone in patients with large skull defects to a certain extent, and meet clinical needs. In order to reduce the rejection reaction, methods such as radiation method and high-pressure steam sterilization are commonly used to treat allograft bone. Because the acquisition of allogeneic materials will cause great trauma to the donor and involve many ethical issues, it has been rarely used at present.
Polymer Materials
Polymethylmethacrylate
This material is strong, stable, heat-resistant, and can be penetrated by X-rays. It is also called bone cement because its strength is similar to that of human bones. However, it is brittle and prone to cracking when impacted by external forces, so it is rarely used alone in cranial repair. Compared with autologous bone, polymethyl methacrylate lacks porosity and cannot be infiltrated and wrapped by new tissue after being implanted in the cranium. It is prone to infection after operation, and it is less used at present. In addition, because it is difficult to be compatible with the surrounding tissue and cannot grow with the skull, it is forbidden to be used as a repair material for children's skull defects.

Hydroxyapatite
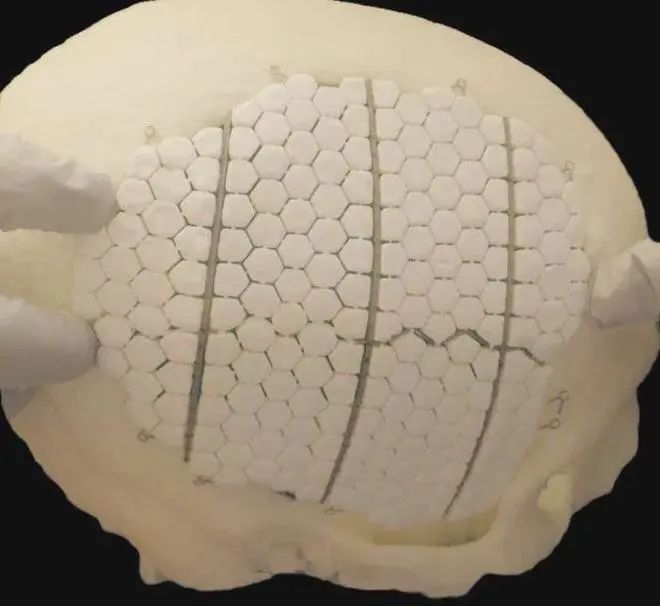
Its molecular structure and calcium-phosphorus ratio are very similar to the inorganic components in normal bones, and it belongs to calcium-phosphorus ceramics. Hydroxyapatite has good biocompatibility, osteoconductivity and osteoinductivity. After implanted in the body, calcium and phosphorus will be released from the surface of the material to be absorbed by body tissues and induce new bone tissue growth. Through CAD/CAM technology, hydroxyapatite can be prefabricated into personalized implants according to the size and shape of the defect before operation, but the main problem is that intraoperative screw fixation and postoperative external force are easy to break it , a higher rate of postoperative infection. Moreover, hydroxyapatite degrades too quickly in the body, so it is usually used to repair small bone defects left by skull drilling, and large skull defects need to be fixed with titanium mesh.
Silicone Rubber
A non-metallic material widely used in cranioplasty at the end of the last century. It has the advantages of easy cutting and fixing, good tissue compatibility, and low price. But its disadvantages are that the material is thicker, the texture is softer, the strength is poor, and the edges are not easy to adhere to and easily warped. The unstable material can easily cause subcutaneous fluid or infection, displacement, upturning and exposure. The use of silica gel for repair is difficult to achieve timely stability and long-term support effects, so silicone rubber is gradually eliminated.

Metal grafting material
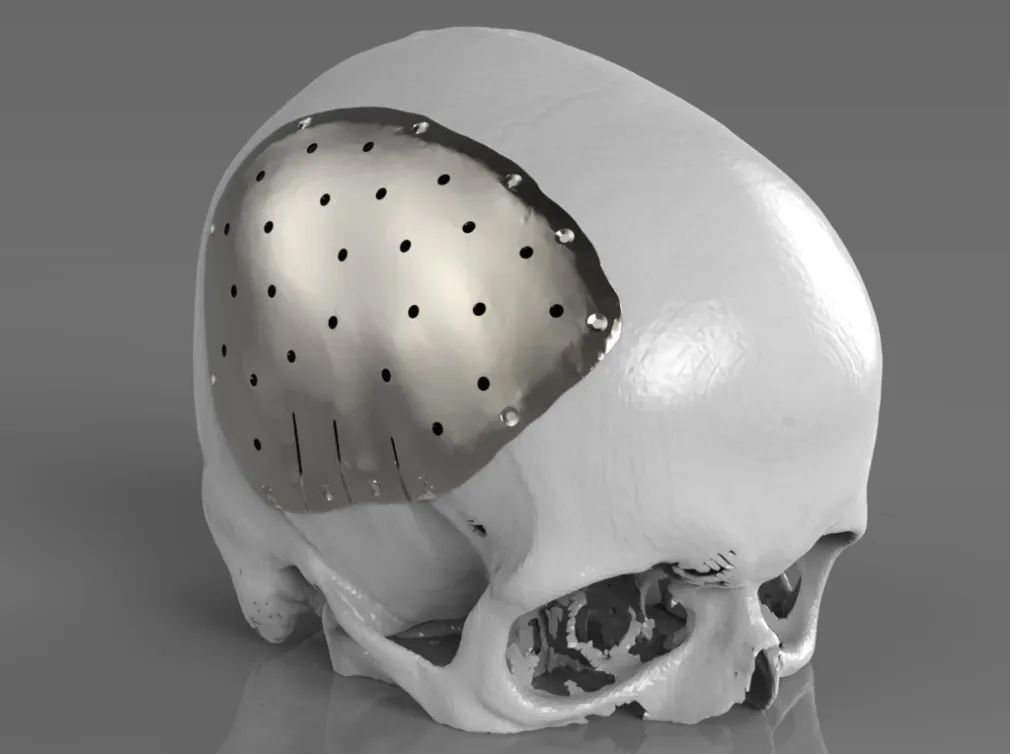
Metals that can be used for cranioplasty mainly include gold, silver, aluminum, titanium, etc. Aluminum is no longer used as a metal material for bone grafts, which dissolves over time and can irritate nerve tissue in the brain and induce epilepsy. Gold, while effective as a restorative material, is not widely used because of its soft texture and not being cost-effective. The skull repaired with silver plates is prone to oxidative reactions with the surrounding skin tissue, causing the skin flap to change color. Moreover, pure silver is soft and has poor resistance to external forces. It deforms after being stressed, thereby damaging intracranial tissues and nerves. Titanium began to be used in cranioplasty in the 1950s. The material made of titanium is safe, high in strength, and strong in acid and alkali resistance, and rarely produces rejection in the human body, so it is currently widely used in clinical practice. However, titanium metal has high brightness in postoperative CT or MRI imaging. If hematoma or tumor occurs near the intracranial implant after surgery, it is difficult to judge on the image. In addition, because titanium is a metal material with good heat transfer properties, it may cause damage to intracranial brain tissue and nerves in an outdoor high-temperature environment. Therefore, titanium metal is still not the most ideal material for cranioplasty.
PEEK
Polyetheretherketone (PEEK), as a semi-crystalline linear polycyclic aromatic linear polymer, was first used in clinical implants in 1998, mainly in spinal and hip replacements, due to its strength, durability Due to the excellent properties exhibited in the combination of toughness, stiffness and resistance, the use in clinical medicine continues to expand. In 2007, the experience of using PEEK material in the reconstruction of fronto-orbital defects in maxillofacial surgery was reported for the first time, making PEEK material gradually recognized by neurosurgeons.

The main advantage of PEEK material is that the elasticity and strength thresholds are very close to those of cortical bone, making it a valuable option for reconstruction of cranial defects. PEEK has the strength and hardness similar to cortical bone, and is highly inert, which basically excludes the release of cytotoxic substances caused by mechanical or chemical decomposition factors. In addition, due to the structural stability of the PEEK material at high temperatures, it can be sterilized by wet or dry heat without deformation. Its extremely low thermal conductivity reduces the possibility of damage to intracranial brain tissue and nerve tissue caused by changes in external temperature, and will not affect the results of imaging examinations of patients. In addition, polyether ether ketone material can also be made into a molding material that is almost identical to the biological curvature of the patient's skull through the combination of CT thin-layer scanning and computer 3D printing technology, making the skull more beautiful after repair. However, the price of polyetheretherketone materials is relatively high, which is difficult for some patients to accept. Therefore, under the premise of not considering the price factor, polyetheretherketone material is considered to be the most ideal material for cranioplasty.
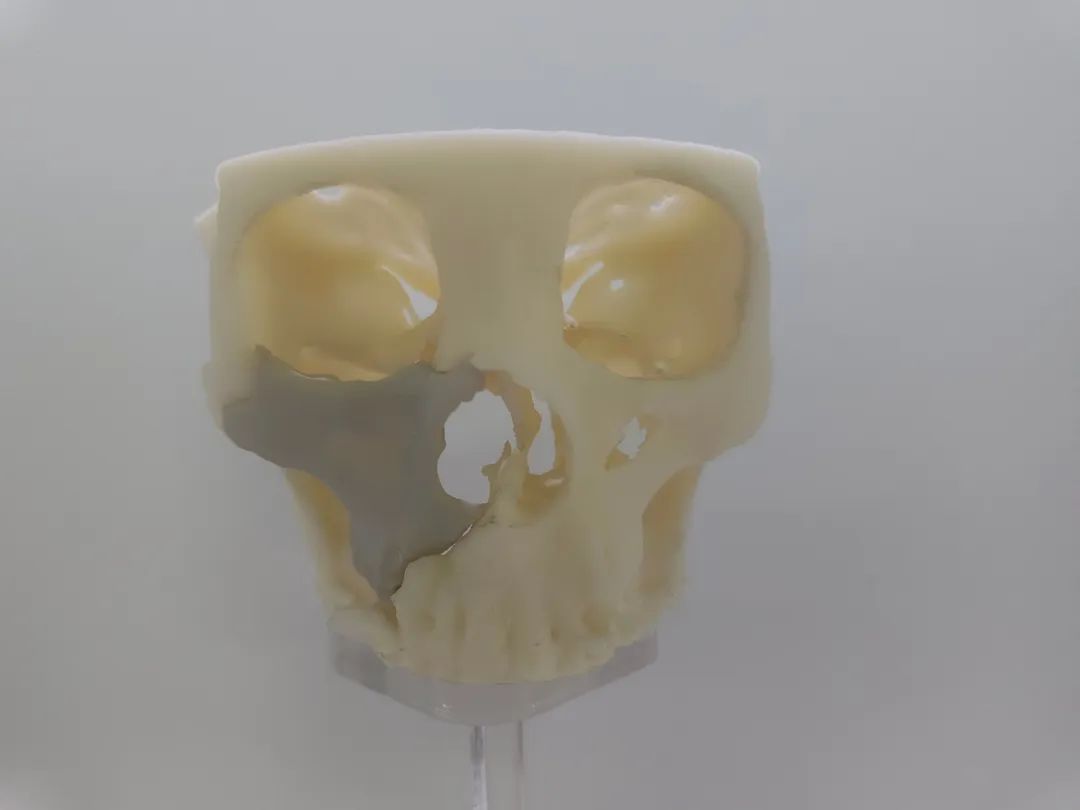
ARKMED ARK-BioPEEK's self-developed and produced medical implant grade polyetheretherketone (PEEK) material has excellent performance and low price, and is suitable for the repair and implantation of skull defects.